Sinusitis and Cystic Fibrosis
by Noreen Henig, MD
Introduction
When one thinks of respiratory disease in cystic fibrosis (CF), it is usually lung disease that comes to mind. However, acute and chronic sinusitis is a common complication of CF that can cause significant symptoms and in some cases may contribute to the worsening of lung disease.1,2,3 Anatomically, the lungs can be thought of as the "lower respiratory tract" while the nares and sinuses can be thought of as the "upper respiratory tract." By evaluating the respiratory tract as one continuous structure, it becomes easier to understand the underlying pathophysiology and treatment of sinus disease in CF.
The Sinuses in Cystic Fibrosis
The sinuses are a group of 4 pairs of air filled spaces in the head. They are called the ethmoid, maxillary, sphenoid, and frontal sinuses. (Fig. 1) The sinuses warm and humidify the air as one breathes. They also trap and filter organic and non-organic particles from the air, such as bacteria, spores, and dust. The sinuses are lined with a layer of epithelium, similar in most ways to the layer of epithelium that lines the lower respiratory tract. It is the respiratory epithelium that is affected by cystic fibrosis, and that leads to the inflammation and infection that causes harm. Most patients with CF suffer from pansinusitis, inflammation and infection of all the sinuses.
"…the great majority of patients with CF develop sinus symptoms…"
The true incidence of sinusitis in CF is not known, but the great majority of patients with CF develop sinus symptoms, usually between the ages of 5 and 14 years.4 Symptoms of sinus disease include:
Adolescents and adults are more likely than children to report headaches, and headaches are often unresponsive to typical headache remedies. Acute sinusitis is the term applied when symptoms become severe, but in reality, patients with cystic fibrosis always have chronic sinusitis.
- nasal obstruction
- chronic congestion or discharge
- headaches
- post-nasal drip with morning cough
- cough that is aggravated by lying down
- severe bad breath
- constant need to "clear one's throat"
While millions of people throughout the world suffer from sinusitis, only a small fraction have CF. There are specific physical and radiographic findings that can distinguish CF related sinusitis from non-CF sinusitis. Nasal polyps are the most distinctive of the physical findings. Polyps are benign masses of extra tissue that cause problems related to their size and location. Nasal and sinus polyps form commonly in CF and can obstruct drainage of the nose and sinuses, and in extreme instances, may even protrude from the nares (nostrils). (Fig. 2)
Figure 2: A view of a maxillary sinus with purulent discharge from the ostium (arrow) and a large, obstructing polyp(P). The physical appearance of polyps in CF is the same as in patients with severe allergy induced sinus disease. However, under the microscope, CF related polyps have fewer eosinophils ( <4 % ) and the mucus glands contain acid rather than neutral mucins.1 The prevalence of nasal polyps in CF has been reported as high as 48% and appears to be proportional to age.5,6
_
"…lack of proper formation, of the frontal sinuses is common in CF…"
Another distinctive feature of CF related sinusitis is how the sinuses look on imaging studies. Plain radiographs, computed tomography (CT) and magnetic resonance imaging (MRI) are all appropriate tools to evaluate patients with sinus symptoms. Agenesis, or lack of proper formation, of the frontal sinuses is common in CF and can be seen on plain radiographs. This finding is thought to be due to obstruction of the sinuses that occurs early in life.7 In CT and MRI scans, more than 75% opacification of the maxillary and ethmoid sinuses is considered a hallmark of CF. Finally, abnormal paranasal sinuses, defined as bulging of the lateral nasal wall near the middle meatus and resorption of the uncinate process (bony structures found in the nose) is considered a finding distinctive for CF sinusitis.8
Since sinusitis is characterized by infection, it is easy to predict that the infections found in CF related sinusitis are distinct from the bacterial infections found in non-CF sinusitis. Just as in lung infections in CF, the most common agents of sinusitis in CF are:
- Staphylococcus aureus
- Haemophilus influenza
- Pseudomonas aeruginosa
- Burkholderia cepacia
- Achromobacter (a.k.a. Alcaligenes or Acinetobacter) xylosoxidans
- Stenotrophomonas maltophilia
Patients with CF can have high bacterial loads in their sinuses without experiencing any symptoms. Non-bacterial infectious agents are also found in CF sinusitis. Aspergillus spp. is thought to colonize sinuses in up to 40% of adults, although its presence is unlikely to cause symptoms. Interestingly, CF patients are no more susceptible to common viral upper respiratory infections (e.g. the "common cold") than non-CF patients. 9
_
"…about 20% of patients with CF will also be allergy-sufferers…"
The role of "hay fever" or allergic rhinitis in CF sinusitis is not entirely clear. The incidence of allergic rhinitis in CF is the same as the general population.10 At this point in time, there is no identified association of allergies contributing to the development of nasal polyps (remember, under the microscope allergic and CF polyps look different) or even the development of asthma or worsened lung disease. However, since about 20% of patients with CF will also be allergy-sufferers, it is important to pay attention to known allergies or seasonal worsening of sinus symptoms to provide better treatment for patients with CF sinusitis.
Diagnosis
Diagnosis of CF related sinusitis is primarily based on symptoms. Since most patients with CF will have abnormal imaging studies like sinus CT scans, imaging studies are used to evaluate the extent of disease and to track any changes with therapy. Bacterial cultures, usually done with nasal swabs or transantral aspirates, can guide antibiotic regimes. Sinus endoscopy, or placement of a small camera into the maxillary and sometimes ethmoid sinuses, can be performed by an otolaryngologist (ears, nose and throat specialist) to evaluate the extent of disease and to visualize sinus polyps. (Fig. 3) Material for microbiologic cultures can be obtained via the endoscope as well.Treatment
Treatment of CF-related sinusitis takes on many forms including:Each of these will be discussed individually, but in general, while there is no consensus on the ‘best’ treatment of CF related sinus disease, most symptomatic patients benefit from a combination of therapies. In addition, most of the modalities available are borrowed from the treatment of chronic sinusitis in non-CF sinusitis patients, and have not necessarily been investigated specifically for use in patients with CF.
- antibiotics
- nasal steroids
- mechanical clearance with saline or antibiotic flushes
- antihistamines and decongestants
- surgical intervention
_
(…patients are infected with the same organism throughout the respiratory tract…)
The role of antibiotics in CF sinus disease is similar to that of CF pulmonary disease. Experimental antibiotic therapy should always consider the array of CF specific pathogens, especially Pseudomonas spp. Nasal swabs and transantral aspirations can give specific information about sinus infections.4 Sputum samples are also quite useful, and it is typical that patients are infected with the same organism throughout the respiratory tract. The ideal length of therapy with sinusitis is not known, although treatment courses of systemic antibiotics tend to be longer due to poor penetration of the antibiotics into the sinuses and decreased ability to do ‘airway clearance’ of the sinuses. The usual duration of therapy is 3-6 weeks.1,11
_
(…nebulizers adapted for inhalation through the nose…)
Antibiotics can be delivered systemically, via mouth or vein, or locally by inhalation or direct installation into the maxillary sinuses. Systemic antibiotics are the standard of care, and usually treat sinus and pulmonary exacerbations simultaneously. Nebulization of antibiotics directly into the sinuses has been studied in a non-CF population. In an 8-week study of non-CF sinusitis, nebulized aminoglycosides were shown to decrease bacterial colonization and inflammation of the nasal cavity.12 It is generally accepted that there is some penetration of the sinuses with TOBI for patients who use the drug regularly. Commercial companies now sell nebulizers adapted for inhalation through the nose and dispense an array of antibiotics for nasal inhalation. Anecdotally, many CF patients have benefited from this form of treatment.
Flushing of the maxillary sinuses through catheters placed directly into the sinus is possible in patients who have undergone surgical antrostomies. In two uncontrolled trials of lung transplant patients, flushing of the sinuses with tobramycin through antrostomies resulted in absence10 or delay2 of contamination of the newly transplanted lungs with Pseudomonas spp. A retrospective study of 32 CF patients with chronic sinusitis showed that those who had monthly flushes with tobramycin had fewer surgeries over a 2-year period of time. 13 What still remains unclear is how this treatment compares to other forms of 'airway clearance' for the upper respiratory tract and what the influence of monthly checks on the sinuses is.
_
(…patients can flush with a buffered saline solution they make themselves…)
Anecdotally, some patients get relief of their sinus symptoms by flushing their nares with saline. Symptomatic improvement is achieved by clearing mucus and hydrating thick secretions. It may also decrease blood flow resulting in decongestion. Of course, infectious organisms are also removed with the nasal secretions. Many patients are asked to do this regularly after endoscopic surgery. Commercially available products include saline-filled squeeze atomizers, some which contain the moisturizing agent glycerol. More economically, patients can flush with a buffered saline solution they make themselves. The nares are washed with the saline using a bulb or catheter-tipped syringe.
Nasal steroids are a mainstay of therapy for non-CF sufferers of sinusitis. They are used with variable success in patients with CF related sinusitis. There are reports that regular use of nasal steroids diminish the size and number of nasal polyps, and that use after polypectomy decreases the rate at which polyps reform.11
No convincing data exists to support the use or disuse of antihistamines and decongestants in CF. Some patients have been counseled to stay away from them for fear of further drying out secretions. Other CF patients, especially those with a clear history of allergies, use antihistamines regularly with relief of symptoms of stuffiness and runny nose and no worsening of their lung congestion. Decongestants, such as pseudoephedrine (Sudafed), can be helpful for relieving symptoms of sinus headache or fullness. Topical decongestants, such as oxymetazoline (Afrin), can give temporary relief by promoting sinus drainage, but should not be used more than three consecutive days for fear of a rebound phenomenon leading to increased nasal secretions. Mucolytics, such as guaifenesin, may be used to promote sinus drainage and are thought not to be detrimental.14
Surgical treatment of sinus disease should be considered in anyone with CF and ongoing nasal or sinus symptoms such as:
The surgical options include placement of antrostomies, debridement of maxillary sinuses, ethmoidectomies, and nasal polypectomy. The surgeries are usually done with an endoscope, a small, narrow cameral inserted into the nares. (Fig. 3) Advanced endoscopic sinus surgery involves use of a CT scanner in conjunction with the endoscope to help the otolaryngologist gain a 3-D view of the sinuses. It provides better access to ethmoid, paranasal and even frontal sinuses. Surgical intervention is shown to relieve nasal obstruction, decrease purulent nasal discharge, increase activity level, and improve olfaction. 15
- headache
- loss of taste or smell
- severe post-nasal drip
- frequently recurring pulmonary exacerbations
- those awaiting lung transplantation1, 1,11
Figure 3: Tools used by the otolaryngologist. a) A transantral aspirator for taking samples from the sinuses for culture. b) The endoscope for viewing inside the maxillary and ethmoid sinuses. 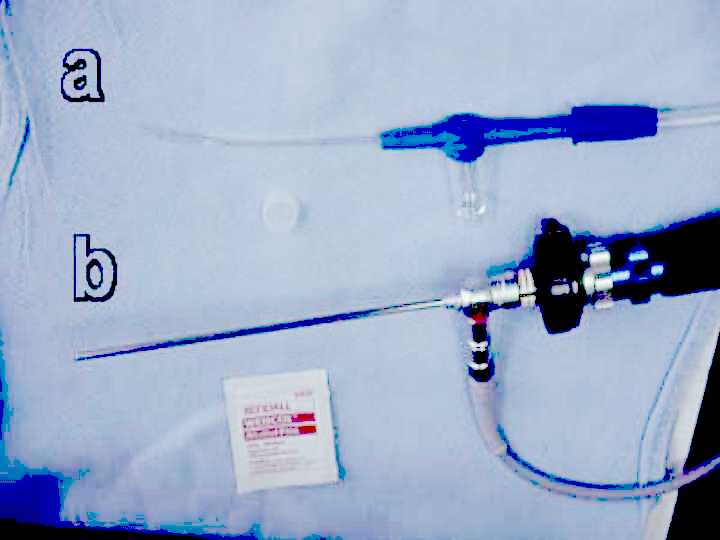
_
(…all patients reported clinical improvement and overall improved sense of well being.)
Antrostomies and ethmoidectomies are usually done as a vehicle to augment medical therapy. This allows direct access to the maxillary sinuses via flexible catheters through which saline or antibiotics can be instilled. In an uncontrolled study of 37 CF transplant patients undergoing antrostomies followed by monthly flushing, all patients reported clinical improvement and overall improved sense of well being.2 Nasal or sinus polypectomy is the treatment of choice for obstructive polyps. With growing experience and newer techniques with endoscopic surgery, recurrence is less frequent.16 Surgery done in childhood does not protect against the development of chronic sinusitis in CF,14 and therefore should be reserved for symptomatic patients who fail medical intervention. In addition, sinus surgery without aggressive follow-up medical care, such as upper airway clearance measures or inhaled corticosteroids, is not useful.17
SUMMARY
Sinus disease is common in children and adults with CF. Symptoms can be quite varied and debilitating, although not life-threatening. There is a wide range of medical and surgical interventions. Most are used with success, although there is a small number of clinical trials, especially those that might compare interventions. Nonetheless, most patients with CF can achieve relief of their sinus symptoms.References
- Ramsey B, Richardson MA: Impact of sinusitis in cystic fibrosis. J Allergy Clin Immunol 90:547-53, 1992.
- Lewiston N, King V, Umetsu D, Starnes V, Marshall S, Kramer M, Theodore J: Cystic fibrosis patients who have undergone heart-lung transplantation benefit from maxillary sinus antrostomy and repeated sinus lavage. Transplant Proc 23:1207-8, 1991.
- Umetsu DT, Moss RB, King VV, Lewiston NJ: Sinus disease in patients with severe cystic fibrosis: relation to pulmonary exacerbation. Lancet 335:1077-8, 1990
- Stern RC, Boat TF, Wood RE, Matthews LW, Doershuk CF: Treatment and prognosis of nasal polyps in cystic fibrosis. Am J Dis Child 136:1067-70, 1982
- Brihaye P, Clement PA, Dab I, Desprechin B: Pathological changes of the lateral nasal wall in patients with cystic fibrosis. Int J Pediatr Otorhinolaryngol 28:141-3, 1994
- Coste A, Gilain L, Roger G, Sebbagh G, Lenoir G, Manach Y, Peynegre R: Endoscopic and CT-scan evaluation of rhinosinusitis in cystic fibrosis. Rhinology 33:152-3, 1995
- Ledesma-Medina J, Osman MZ, Girdany Br: Abnormal paranasal sinuses in patients with cystic fibrosis of the pancreas. Pediatr Radiol 9:61-6, 1980
- Nishioka GJ, Cook PR, McKinsey JP, Rodriguez FJ: Paranasal sinus computed tomography scan findings in patients with cystic fibrosis. Otolaryngol Head Neck Surg 114:394-9, 1996
- Ramsey BW, Gore EJ, Smith AL, Cooney MK, Redding GJ, Foy H: The effect of respiratory viral infections on patients with cystic fibrosis. Am J Dis Child 143:662-8, 1989
- Davidson TM, Murphy C, Mitchell M, Smith C, Light M: Management of chronic sinusitis in cystic fibrosis. Laryngoscope 105:354-8, 1995
- Hui Y, Gaffney R, Crysdale WS: Sinusitis in patients with cystic fibrosis. Eur Arch Otorhinolaryngol 252:191-6, 1995
- Kobayashi T, Baba S: Topical use of antibiotics for paranasal sinusitis. Rhinology 14:77-81, 1992
- Moss RB, King VV: Management of sinusitis in cystic fibrosis by endoscopic surgery and serial antimicrobial lavage. Reduction in recurrence requiring surgery. Arch Otolaryngol Head Neck Surg 121(5):566-72, 1995
- Marks SC, Kissner DG: Management of sinusitis in adult cystic fibrosis. Am J Rhinol 11(1):11-4, 1997
- Nishioka GJ, Barbero GJ, Konig P, Parsons DS, Cook PR, Davis WE: Symptom outcome after functional endoscopic sinus surgery in patients with cystic fibrosis: a prospective study. Orolaryngol Head Neck Surg 113:440-5, 1995
- Rowe-Jones JM, Mackay IS: Endoscopic sinus surgery in the treatment of cystic fibrosis with nasal polyposis. Laryngoscope 106:1540-4, 1996
- Mak GK, Henig NR. Sinus disease in cystic fibrosis. Clinical Reviews in Allergy and Immunology 21: 51- 63, 2001.