Dementia in Huntington's Disease
Dementia refers to neurodegeneration that results in loss of mental abilities. Neurodegeneration is the loss of mental abilities that can be caused by brain damage and/or neuron death. For this reason, dementia is common in neurodegenerative disorders such as Alzheimer’s Disease. While Huntington’s Disease (HD) is commonly thought of as a motor disorder, cognitive symptoms can be present which can progress to dementia. To learn more about some of these cognitive symptoms, click here. Interestingly, many cognitive symptoms appear in HD patients before motor deficits appear.
Although a formal clinical diagnosis of HD depends on unequivocal signs of motor impairment, recent research has shown the importance of neuropsychological analysis and the evaluation of dementia in determining the condition of HD patients. There are several tests that clinicians administer to evaluate a patient’s cognitive abilities and degree of dementia. For physicians, it is important for these tests to recognize the subtle differences between different neurodegenerative diseases, particularly HD, Alzheimer’s disease and Parkinson’s Disease, which show similar cognitive symptoms.
Testing for Dementia^
When dementia is suspected in patients, physicians will administer tests before giving a formal diagnosis. For patients, whether they are at risk for HD or other diseases associated with dementia, the Mini-Mental State Examination (MMSE) is the most common test that is administered. The MMSE is convenient to administer to patients because it is relatively short, but can still help determine whether a patient’s cognitive functions are declining.
In addition to the MMSE, physicians also use other neuropsychological tests that usually involve several mental tasks that require the use of different areas of the brain. For example, the striatum, the brain area most affected in HD, has been implicated in sequence and procedure learning. Since the neuropsychological tasks test different regions of the brain, physicians can use the results to determine what regions of the brain have been affected. When patients are tested for dementia using these tests, their performance is compared to that of healthy individuals on the same tasks. Researchers are still determining which neuropsychological tests are most suitable for evaluating certain regions of the brain.
How are dementias classified?^
After a patient is diagnosed with dementia, it is important to determine the kind of dementia that is present. Dementias are often classified by the region of the brain that is affected. One of the main classifications divides dementias into two main groups: cortical and sub-cortical based on the area of the brain where degeneration occurs. The cortical region consists of the cerebral cortex while the sub-cortical region is comprised of the other structures of the brain including the thalamus, hypothalamus, cerebellum and brain stem (See Figure 1). To learn more about the brain click here for the HOPES Brain Tutorial. Whether cortical and subcortical dementias should be considered separately is still controversial among researchers and physicians. In general, studies have shown that some differences do exist, but there is disagreement on the degree to which the two dementias differ.

Figure 1: The brain can be divided into the cortical and subcortical regions. The cortical region consists of the cerebral cortex while the sub-cortical region consists of the thalamus, hypothalamus, cerebellum and brain stem.
To more clearly define the two types of dementia, researchers have studied whether their effects on memory differ. Alzheimer’s patients are often used as a model for cortical dementia because patients with this disease have large amounts of degeneration in the cerebral cortex. Clinical studies of Alzheimer’s patients have shown that cortical dementias have difficulty performing tasks that require semantic memory. Semantic memory is what we use to store facts without respect to the setting where we learned the facts (See Figure 1). To evaluate this type of memory, patients are asked to perform tasks such as matching pictures and generating definitions of words. To a lesser degree, cortical dementia can also affect episodic memory, which is used to remember experiences and the setting in which facts are learned. For example, after a boy bumps his head in a bike accident, semantic memory would enable him to remember that wearing a helmet is important when riding bikes, while episodic memory would enable him to recollect the specific time when the accident occurred.
Sub-cortical dementias have a slightly different effect on memory than cortical dementias in that they have a smaller effect on semantic memory. HD and Parkinson’s disease are considered sub-cortical dementias. In HD, patients instead find it challenging to accomplish cognitive tasks that require retrieval and synthesis of known facts, such as forming abstractions. Unlike patients with Alzheimer’s, however, those with HD can accomplish tasks that require semantic memory under the right conditions. For example, one study tested patients on a category fluency task in which patients were asked name as many items as possible from certain categories (e.g. foods, animals, plants) within an allotted time period. Under what scientists call “cued” conditions in which patients were given hints or clues that help with the task, HD and Parkinson’s patients improved their scores. Alzheimer’s patients, however, did not perform better under “cued” conditions. This suggests that patients with HD or other types of sub-cortical dementia have not experienced degradation of semantic memory per se, but instead have difficulty retrieving facts from their memory.
Sub-cortical dementias like HD do not affect memory following a time-dependent gradient. Memories and knowledge obtained recently are not more susceptible to degeneration than those from the distant past, as is the case in Alzheimer’s Disease. To learn more about the effects of HD on memory click here.
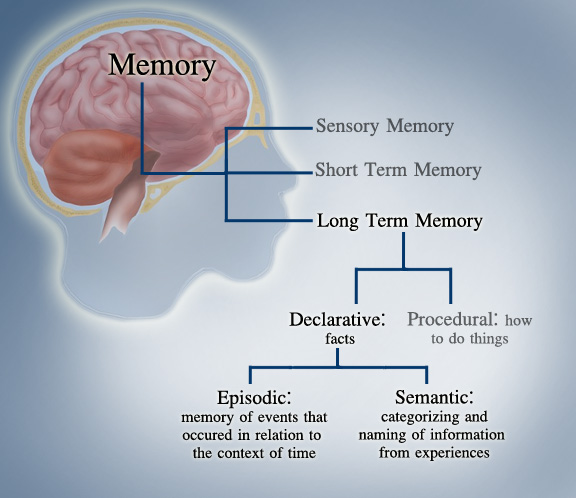
Figure 2: Our brains use different types of memory. Cortical dementia is thought to affect semantic memory to a greater degree than episodic memory. Sub-cortical dementia, as in HD, is thought to affect semantic memory to a lesser degree than cortical dementias.
Although memory is one of the leading areas of interest in the study of cortical and subcortical dementias, other differences between the two dementias exist. Sub-cortical dementias almost always result in motor disorders. Chorea in HD patients and tremors in Parkinson’s tremors are examples of motor impairment that accompany sub-cortical dementias. In terms of other cognitive effects, differences between dementias are still being studied.
Criticisms of the Dementia Differentiation^
Some researchers and physicians consider the differentiation between cortical and sub-cortical dementia important for patient diagnosis, but others remain skeptical that a significant difference exists. The major criticism of the studies that show variation between cortical and sub-cortical dementias is that there is pathological overlap between the sample groups that are used to model the two categories. These studies often assume that Alzheimer’s patients mostly have cortical dementia and HD or Parkinson’s patients preferentially exhibit subcortical dementia. Necropsies have shown, however, that the brains of both Alzheimer’s and HD patients exhibit a certain degree of both categories of dementia.
If in fact both cortical and subcortical dementia occur in Alzheimer’s, HD, and Parkinson’s patients, then these studies may be problematic. As a result, physicians are still trying to learn more about the differences between the pathologies of the diseases in hopes of finding a more reliable way of differentiating dementias. The ability to differentiate dementias may lead researchers and physicians to better diagnose and treat neurodegenerative diseases.
Further Reading^
- Langbehn, Douglas R. et al. “Predictors of diagnosis in Huntington disease.” Neurology. 2007; 68: 1710-1717.
Researchers and The Huntington Study Group performed a longitudinal study to identify early clinical symptoms that arise in HD patients. Findings showed that psychological performance can be used in diagnosis along with motor impairment. There is a thorough discussion of clinical evaluation of neurological performance in HD patients and the types of tests administered to patients. - Rosser, Anne and John R. Hodges. “Initial letter and semantic category fluency in Alzheimer’s disease, Huntington’s disease and progressive supranuclear palsy.” Journal of Neurology, Neurosurgery and Psychiatry 1994; 57: 1389-1394.
This study examined symptoms related to semantic and episodic memory in three different neurodegenerative diseases. Several neuropsychological tests were administered to patients and the results suggested that semantic memory is more heavily influenced in cortical dementias like Alzheimer’s disease. - Sadek, Joseph R. et al. “Retrograde Amnesia in Dementia: Comparison of HIV-Associated Dementia, Alzheimer’s Disease, and Huntington’s Disease.” Neuropsychology, 2004; 18.4: 692-699.
This study tested how three different types of dementia affect memory. The findings show that overall dementia is equally severe in all three types, but memory impairment differs. Time-dependent memory loss was not found in HD patients and HD patients were able to improve on memory tasks under “cued” conditions. The authors discuss their findings in the context of the debate on how cortical and subcortical dementias differ. - Wedderburn, C et al. “The utility of the Cambridge Behavioural Inventory in neurodegenerative disease.” Journal of Neurology, Neurosurgery, and Psychiatry. 2008; 79: 500-503.
A review of a new test that is used to evaluate the mental condition of patients with neurodegenerative diseases. It includes helpful information about cognitive and psychological symptoms in HD, Parkinson’s and Alzheimer’s patients and how these symptoms differ between the diseases.
Additional Resources:
- Ho AK, Sahakian BJ, Brown RG, Barker RA, Hodges JR, Ane MN, Snowden J, Thompson J, Esmonde T, Gentry R, Moore JW, Bodner T (2003) “Profile of cognitive progression in early Huntington’s disease.” Neurology 61:1702-1706.
- Kirkwood SC, Siemers E, Hodes ME, Conneally PM, Christian JC, Foroud T (2000) “Subtle changes among presymptomatic carriers of the Huntington’s disease gene.” J Neurol Neurosurg Psychiatry 69:773-779.
- Lawrence A, Hodges J, Rosser A, Kershaw A, French-Constant C, Rubinsztein D, Robbins T, BJ S (1998) “Evidence for specific cognitive deficits in preclinical Huntington’s disease.” Brain Pathol 121:1329-1341.
- Lemiere J, Decruyenaere M, Evers-Kiebooms G, Vandenbussche E, Dom R (2004) “Cognitive changes in patients with Huntington’s disease (HD) and asymptomatic carriers of the HD mutation—a longitudinal follow-up study.” J Neurol 251:935-942.
- Meade, Catherine E. “Diagnosing Dementia: mental status testing and beyond.” Australian Prescriber, 2005 (28): 11-13.
- Savla, Gauri Nayak and Barton W. Palmer. “Neuropsychology in Alzheimer’s disease and other dementia research.” Current Opinions in Psychiatry, 2005 (18): 621-627.
– T. Wang, 5/17/09
