HPV and Cervical Cancer
http://web.uct.ac.za/depts/mmi/jmoodie/hpv.html
Prevalence of
Cervical Cancer
Cervical cancer is the third most common cancer
among women worldwide with 400,000 newly diagnosed cases every year. Cervical cancer
is the most common cancer of women in most developing countries, where it
accounts for as many as one in four female cancers. It occurs much less
frequently in developed countries. In the US, there are about 15,000 new
diagnosed cases each year and about 1/3 of these women die of the malignant
form of the disease. This incidence in women in the US varies among ethnic
groups; it is twice as prevalent in black women than in white women. Cervical
HPV infection is extremely common in sexually active young women. Peak
prevalence is seen between 15 to 25 years of age and varies from 25 to
40%.
Prevalence of
HPV
Information
on HPV prevalence worldwide is inconsistent since there is no standardized
method of detection. There is virtually no data on HPV prevalence in developing
countries. Many people infected with HPV may not develop symptoms for several
months or have access to health care facilities. An estimated 60% of HPV
prevalence depends largely on the accuracy of the detection methods.
http://www.brown.edu/Courses/Bio_160/Projects1999/hpv/epidem2.html
Cervical
cancer facts
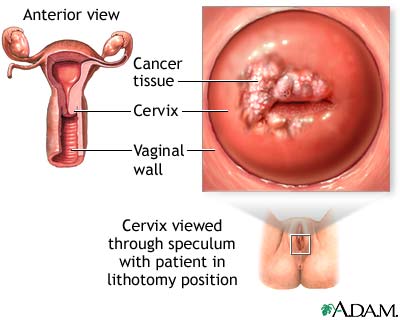
¤
Most
cancers occur in the transformation zone of the cervix, where the columnar
cells of the endocervix form a junction with the stratified squamous epithelium
of the exocervix. About 85% of
cervical cancers are squamous cell cancers. Most other cases are
adenocarcinomas.
¤
Lesions
that are destined to become maliganant squamous cell carcinomas usually undergo
a series of dysplastic changes over a time span of many years. The severity of
the dysplasia is rated by the degree to which the squamous epithelium is
replaced by basaloid cells, where the most severe dysplasia has the entire
thickness displaced. Most dysplasias do not progress and resolve spontaneously.
¤
A
world-wide study of almost 1,000 cervical cancers indicated that more than 90%
contain HPV DNA. Although more than 20 types were found in the tumors, four
types (HPV-16, HPV-18, HPV-31, and
HPV-45) accounted four about 80% of the HPV-positive cancers.
¤
HPV-16
appears to be the most common type of HPV found in cervical cancers. HPV-18 is
the predominant type in adenocarcinomas, and HPV-16 is the most common type in
squamous cell cancers.
¤
In
mildly dysplasic lesions, each of the ORFs appears to be expressed, mainly in
the upper layers of the epithelium, but in high grade dysplasias, a more
restricted number of ORFs are expressed, primarily E6 and E7, and their
expression is found primarily in the basal, proliferating layer of the
epithelium.
Road to
Cervical Cancer
Although infection with HPV is raises the risk
of developing cervical cancer and may be necessary for the development of
cervical cancer, it is clearly not sufficient. Other factors must collaborate
to cause oncogenesis. Some changes can be virus specific: e.g. viral
integration into the host genome leading to decreased expression of some viral
genes; increased expression of E6 and E7; and selective growth advantage. Other
alterations include genetic alterations of cellular genes. Tumors typically
have several cellular alterations that lead to loss or gain of function of some
genes involved in growth and cell-cycle regulation. There are also
environmental risk factors, such as smoking or immunosuppression, which
contribute to the development of cervical cancer.