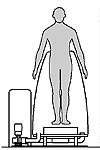
Investigators: Charles G. Burgar, MD and Robert T. Whalen, PhD Project Staff: Douglas F. Schwandt, MS; Ellie L. Buckley, MS PT; Yang Cao, MB; James H. Anderson, JEM; and Vickie Dvonch, MD Project Categories: Stroke / Arthritis - 2000 Early ambulation after neurological injury or orthopaedic surgery can be beneficial, but falls can result if balance or motor strength is lacking. Conditions such as muscle atrophy, sensory loss, or pain may impair the ability of patients to control weight bearing. Previous techniques for partial body weight support (BWS) during gait training have significant disadvantages. We proposed to clinically evaluate a method that was developed at the Gravitational Research Branch of NASA-Ames Research Center to facilitate exercise in space or to simulate microgravity on Earth. By creating a difference in air pressure between body segments above and below the waist, a force acting near the body's center of mass can be created during treadmill ambulation. A clinical version for differential pressure walking assistance (DPWA), developed at the VA Rehab R&D Center, provides BWS similar to that experienced while wading in waist-deep water. Unlike aquatic therapy, the lifting force is continuously variable from 0 to 100% of body weight, is under computer control, and there is no appreciable viscous drag. Hypotheses: 1) The physiological effects of treadmill ambulation using DPWA are predictable and well-tolerated, 2) lower limb loading can be controlled predictably while ambulating using DPWA, and 3) Gait training using DPWA improves function in patients with neurological and orthopedic impairments who require weight support to walk. Findings to Date: In Phase 1, we measured the cardiovascular response of subjects walking with, and without, DPWA. We recruited subjects with medical conditions typical of older rehabilitation patients. Nine subjects were tested without incident. Sessions typically lasted 3 hours and included monitoring physiological parameters during conditions of rest, walking without lower body positive pressure (LBPP) and walking with LBPP at 25, 50 and 75% BWS. Walking with 75% BWS led to significantly (paired t-tests, P<.05) lower heart rate, lower Borg exertion scores, and higher MAP associated with an increased diastolic blood pressure. All subjects tolerated the testing without incident or clinically significant change. Anthropometric data and ground reaction force data were also collected and pooled with subjects in Phase 2. In Phase 2, 10 healthy subjects with a wide range of height and weight were studied to identify the contributions of anthropometric dimensions in determining the pressure requirements for BWS. An average of 0.91 p.s.i. (S.E. ±0.11) provided 75% BWS. Height had a small effect on the amount of pressure needed for BWS. The vertical component of the ground reaction force (GRF) was measured using the Pedar Insole System. When compared to walking without BWS, GRF was reduced by an average of 22.5 % (±5.73) while walking with 25% BWS, 41.9 % (±5.40) while walking with 50% BWS; and by 65.9 % (±7.96) while walking with 75% BWS. Phase 3 is in progress. Publications and Presentations: Burgar CG, Robotics and assisted movement: Assessing, correcting, and compensating for motor impairment. VA/PVA National MS Conference, Chandler, AZ, Feb 4-5, 1999. Buckley EL, Burgar CG, Cao Y, Schwandt DF: Partial body weight support using air pressure: Safety and unloading. Proc 2nd National VA Rehab R&D Conf, Arlington, VA, Feb. 20-22, p. 200, 2000. Funding Source: VA RR&D Merit Review |